Slipped Disc Treatment – Lower Back
 A herniated disc, also known as a slipped disc, disc prolapse or disc rupture, is a common condition that can be painful and debilitating. Intervertebral discs don’t really “slip”—although the phrase “slipped disc” is a popular term to refer to bulging, ruptured, or herniated discs.
A herniated disc, also known as a slipped disc, disc prolapse or disc rupture, is a common condition that can be painful and debilitating. Intervertebral discs don’t really “slip”—although the phrase “slipped disc” is a popular term to refer to bulging, ruptured, or herniated discs.
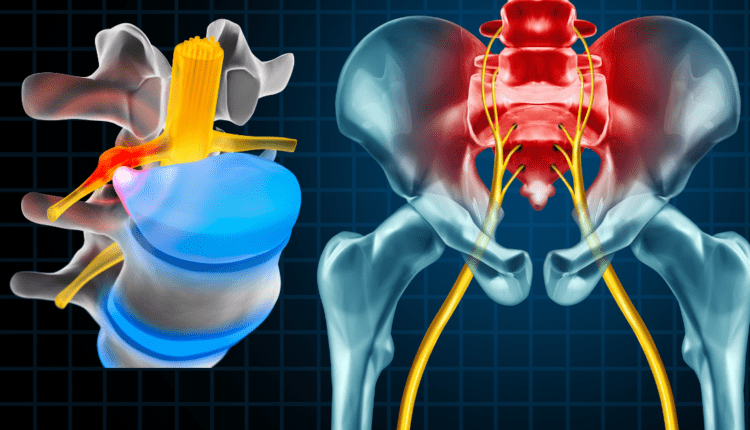
Between each bone of the spine is a disc. The discs are pads that serve as “cushions” between the vertebral bodies. They act to minimize the impact of movement on the spinal column. The discs are made up of a tough outer layer (the annulus fibrosus) and a soft inner layer (much like a jelly donut) called the nucleus pulposus. The nucleus pulposus contains a soft, gelatin-like material.
A herniated disc refers to a problem with one of the rubbery cushions (discs) between the individual bones of the spine (vertebrae). As the disc degenerates from age or injury, the fibrous outer ring (annulus fibrosus) can develop cracks and areas of weakness. This can allow the softer central portion to rupture (herniate) through the outer ring. This abnormal rupture of the central portion of the disc is referred to as a disc herniation (or a “slipped disc”).
The most common location for a herniated disc to occur is between the fourth and fifth lumber vertebrae in the low back. This area is constantly absorbing the impact of weight bearing and load forces on the lower back. Standing or sitting actually increase the load on the L4-L5 disc. The lower back is also involved in bending and twisting motions, making it extremely vulnerable to injury.
Risk factors
Herniated discs can happen at any age, but are more common in people from 35 to 55 years of age. They also occur more frequently in men than women.
Factors that increase the likelihood include:
- Weight: Being overweight puts additional stress on the lower back
- Age: Wear and tear will cause the disc to lose some of the jelly like material (nucleus pulposis)
- Sedentary Lifestyle: causes muscle weakness and stiffness
- Occupation: Individuals with physically demanding jobs involving pushing, pulling, or twisting
- Improper Lifting: A sudden strain from improper lifting, especially while bending and twisting at the waist while lifting.
- Sport Injuries: Sports involving extreme movements or contact can cause herniated discs.
Herniated Discs Are Not Always Painful
A damaged or diseased disc does not always cause pain or any symptoms, at all. In fact, a relatively high percentage of the population over the age of 40 has some sort of disc problem that is found incidentally on an MRI scan. Often the disc herniation has been there for quite some time and only became identified when a patient went in for another problem not involving back pain.
In addition, the severity of the disc problem that is on an MRI scan does not correlate to the amount of pain or symptoms the patient experiences. For example:
- One person with a large herniated disc may have no symptoms, particularly, if the disc does not place pressure on any of the nerves.
- Another individual with a small, almost insignificant disc herniation can suffer burning, searing pain that radiates down the leg.
One study on symptom-free volunteers found that 50 percent had some degree of herniated disk that did not cause them any discomfort
If symptoms do occur, they can include:
- Numbness and tingling in the buttocks or down the leg to the foot
- Weakness in the leg muscles
- Pain in the back that can travel to the buttocks, thighs, calves, and, possibly, the feet. This is often referred to as sciatica because the pain travels along the path of the sciatic nerve.
Diagnosing a Herniated Disc
Making the diagnosis of a herniated disc always begins with a complete history of the problem and a physical examination. The main questions your doctor will be interested in are:
- Did you have an injury?
- Where is the pain?
- Do you have any numbness?
- Do you have weakness in your legs?
- Have you had this problem before?
- Have you had any unexplained weight loss, fevers, or illnesses recently?
Your doctor will also want to know if you have increased pain when you have to urinate or have a bowel movement or if you suddenly suffer from incontinence. If you do, this may be an emergency, and require immediate surgery.
However, the following diagnostic tests will help with the final diagnosis of a herniated disc:
- X-ray — X-rays can indicate “wear and tear” (degeneration) of the spine and possible narrowing of the disc space. However, they do not reveal disc herniations.
- MRI or CT scan — Magnetic resonance imaging (MRI) and computed tomography (CT) scans can show narrowing of the spinal canal caused by a herniation and identify severity of the herniation. The best scan to identify a disc herniation is the MRI.
- CT Myelogram — Sometimes an MRI does not tell the entire story and your doctor may also suggest a CT Myelogram. This is an injection of dye into the spinal canal followed by a CT scan. A myelogram can help pinpoint the size and location of the herniation.
- EMG (electromyelogram) — An EMG may be used in conjunction with the above two tests. This test involves placing small needles into various muscles and measuring electrical activity. The muscle’s response indicates the degree of nerve activity. An EMG can help determine which nerve root or roots are being affected by the disc herniation.
Treatment
Herniated discs can be painful, but the right treatment can relieve symptoms. Most people who experience a mild disc herniation will recover within 4 weeks of the proper treatment.
Various treatment options include medication, Injections, Non-surgical spinal decompression, chiropractic treatment, physical therapy, and surgery.
Medication
![Slipped Disc Pain Medication San Antonio]() Over-the-counter medication (OTC): Ibuprofen- or naproxen-based drugs can help with mild to moderate pain. These should be used only short term. Chronic long term use can cause kidney disease.
Over-the-counter medication (OTC): Ibuprofen- or naproxen-based drugs can help with mild to moderate pain. These should be used only short term. Chronic long term use can cause kidney disease.- Nerve pain medications: Medications for treating nerve pain include gabapentin (Neurontin™), pregabalin (Lyrica™), duloxetine (Cymbalta™), and amitriptyline (Elavil™). One should be aware that these medications merely mask the pain. Long term use can result in a greater degree of nerve damage.
- Narcotics: Codeine, an oxycodone-acetaminophen combination, or another type of narcotic can be prescribed if OTC medications do not relieve discomfort. Side effects include nausea, sedation, confusion, and constipation. Narcotics are highly addictive and should only be used in cases of severely debilitating pain.
- Cortisone injections: These can be injected directly into the troubled area to help reduce inflammation and pain. Steroid medications should be used sparingly because of their adverse effects.
- Muscle relaxants: These help reduce muscle spasms. Dizziness and sedation are common side effects.
Epidural Steroidal Injections (ESI)
 A technique in which corticosteroids and a local anesthetic are injected into the epidural space around the spinal cord. The goal of these injections is to decrease inflammation and pain.
A technique in which corticosteroids and a local anesthetic are injected into the epidural space around the spinal cord. The goal of these injections is to decrease inflammation and pain.
Risks & Side Effects:
- Nerve Damage
- Increase in pain
- Elevated Blood Sugar (glucose)
- Dural Puncture
- Infection
- Bleeding
- Stomach ulcers
A conservative analysis reports that at least 50% of patients will experience pain relief.
Spinal decompression
Non-surgical spinal decompression was originally developed in the 1980’s by Dr Allen Dyer, a medical doctor from Canada. Spinal Decompression Therapy involves stretching and tractioning of the spine, using a computerized and motorized device. This procedure is called Non-Surgical Spinal Decompression therapy (as opposed to surgical spinal decompression, such as laminectomy and microdiscectomy).
In nonsurgical spinal decompression therapy, the spine is stretched, tractioned and relaxed intermittently in a controlled manner. The theory is that this process creates a negative intradiscal pressure (pressure within the disc itself), which is thought to have two potential benefits:
- Pulls the herniated or bulging disc material back into the disc
- Promotes the passage of healing nutrients, into the disc and fosters a better healing environment.
The goal is to draw the disc back in and alleviate pressure from the nerve in order to relieve back pain and/or leg pain.
Contraindications for Spinal Decompression Therapy
The following groups of people are not good candidates for non-surgical spinal decompression:
- Pregnant women
- Patients with broken vertebrae
- Patients who have had spinal fusion
- Patients who have an artificial disc, or other implants, in their spine
- Patients with failed back surgery
- Anyone who has had multiple surgeries without recovery (pain improvement)
Chiropractic Care
 It has long been debated whether or not chiropractic care is safe and appropriate for the treatment of a herniated disc. A new study confirms the vast majority of patients with lumbar disc herniations can find relief with chiropractic care. The findings show that 90% of patients report substantial improvements within three months of receiving their first chiropractic adjustment.
It has long been debated whether or not chiropractic care is safe and appropriate for the treatment of a herniated disc. A new study confirms the vast majority of patients with lumbar disc herniations can find relief with chiropractic care. The findings show that 90% of patients report substantial improvements within three months of receiving their first chiropractic adjustment.
The following chiropractic techniques may be used for the treatment of herniated discs:
- Flexion-Distraction Technique – This technique involves the use of a specialized table that gently “distracts” or stretches the spine. This allows the chiropractor to isolate the affected area while slightly “flexing” the spine using a pumping rhythm.
- Pelvic Blocking Techniques – Pelvic blocking treatments include using cushioned wedges, which are placed under each side of the pelvis. This will allow changes in mechanics to draw your disc away from the nerve it may be pressing on.
- Deep Tissue Massage (DTM) – There are many different types of massage, but deep tissue massage is the best option to relieve deep muscle tension and spasms. These spasms develop to prevent further compression on the nerve in the affected area. DTM should never be used in an acute phase of disc herniation (within the first 2 weeks) as it can actually make the pain worse during this period.
- Hot and Cold Therapy: Hot and cold therapies offer a diversified set of benefits:
-
Cold Therapy or cryotherapy is used to treat acute injuries of your musculoskeletal system. Use of cryotherapy (ice packs or ice massage) reduces inflammation, circulation, muscle, swelling, spasms and pain.
-
Heat Therapy dilates blood vessels of the muscles surrounding the lumbar spine (low back) allowing increased oxygen and nutrients to reach the muscles. This aids in healing the damaged tissue, The increased blood flow removes waste byproducts from muscle spasms allowing the muscles to relax.
- Interferential Current Therapy (IFC) – Interferential current therapy is an effective therapy option used by many chiropractic clinics to relieve pain and accelerate the self-healing process. The high frequency signals of an IFC penetrate through the skin into deeper lying muscle tissues and transmits electrical impulses in minute quantities through your skin. Underlying tissue and nerves are stimulated which to facilitate healing.
Physical Therapy
 The main focus of physical therapy for a herniated disc is to provide pain relief, followed by muscle strengthening and conditioning to prevent further injury.
The main focus of physical therapy for a herniated disc is to provide pain relief, followed by muscle strengthening and conditioning to prevent further injury.
Once the pain from a herniated disc has subsided, Physical therapy often plays a major role in herniated disc recovery. The main goal is to strengthen the core and back muscles allowing for better back support and increased flexibility. Although this will not correct the herniated disc, it will minimize the potential for a flare-up
Types of Physical Therapy Treatments:
- Deep Tissue Massage (DTM) – (see description above)
- Hot and Cold Therapy – (see description above)
- Hydrotherapy- Passive hydrotherapy may involve simply sitting in a whirlpool bath. Hydrotherapy gently relieves pain and relaxes muscles. Active hydrotherapy may involve water aerobics to help condition your body without unnecessary stress.
- Transcutaneous electrical nerve stimulation (TENS): A TENS machine uses an electrical current to stimulate your muscles. Although the treatment is more superficial than IFC treatment, TENS reduces muscle spasms and is believed to trigger the release of endorphins, which are your body’s natural pain killers.
- Core Stability – Your core (abdominal) muscles help your back muscles support your spine. When your core muscles are weak, it puts extra pressure on your back muscles. Your physical therapist may teach you core stabilizing exercises to strengthen your back.
- Flexibility – Learning proper stretching and flexibility techniques will prepare you for aerobic and strength exercises. Flexibility helps your body move easier by warding off stiffness.
- Muscle strengthening: Strong muscles are a great support system for your spine and help prevent future injuries or flare-ups.
Surgery
 Surgery should always be the last resort for a herniated disc. The only exception to this rule is if a person is experiencing bowel or bladder incontinence as a result of the disc herniation. This condition, also known as Cauda Equina Syndrome, may require immediate surgery in order to prevent paralysis. For cases of herniated disc, without incontinence, it is best to try other less invasive modes of treatment.
Surgery should always be the last resort for a herniated disc. The only exception to this rule is if a person is experiencing bowel or bladder incontinence as a result of the disc herniation. This condition, also known as Cauda Equina Syndrome, may require immediate surgery in order to prevent paralysis. For cases of herniated disc, without incontinence, it is best to try other less invasive modes of treatment.
50% of all low back surgeries fail. This statistic is so high that the medical profession has aptly named it as Failed Back Surgery Syndrome (FBSS). This term is used for patients who have had no improvement after surgery or are whose symptoms are worse after surgery. Another research study found that of the 50% of successful low back surgeries (symptoms improved or abated) up to 36% of those patients would then relapse into recurrent back or leg pain symptoms, 2 years later. In many cases, the symptoms were worse than before surgery. All in all, the final success of a low back surgery (of any type) is a mere 14% – 2 years after surgery. For this reason alone, surgery should be used as a last resort after having tried Non-surgical spinal decompression, chiropractic care and physical therapy.
Types of Low Back Surgery:
- Laminectomy – This is a surgical procedure that removes the back of one or more vertebrae allowing access to the spinal cord. The intent is to relieve pressure on nerves. This procedure leaves the low back in a permanent state of weakness and instability leading to further problems down the line, including the possibility of a second surgery.
- Discectomy/Microdiscectomy – Discectomy is the most common surgery used for herniated disc in the lumbar spine. In this procedure, the portion of the diskc -or the entire disc- is removed to alleviate the pressure on your nerve root. Although this may alleviate the pain, it will lead to advanced degeneration of the lumbar spine.
- Spinal Fusion – General anesthesia is required for spinal fusion. In this procedure, two or more vertebrae are permanently fused together. This may be accomplished with bone grafts or it may involve metal or plastic screws and rods inserted into the spine. This will permanently immobilize the portion of your spine it is inserted in. It will decrease your mobility, flexibility, and activity level. This surgery also predisposes you for future injury and advanced degeneration.
In working with herniated disc conditions for the past 25 years, we have found the most effective treatment for the repair of the herniated disc is Non-Surgical Spinal Decompression. This treatment is non-invasive, painless and highly effective. We have found that it offers the quickest recovery time and the highest success rates with preventing reoccurrence.
References
- Ramos G, Martin W. Effects of vertebral axial decompression on intradiscal pressure. Journal of Neurosurgery 81:350-353, 1994.
- Wang G. Powered traction devices for intervertebral decompression: Health technology assessment update. Washington Department of Labor and Industries, June 14, 2004.
- Daniel DM. Non-surgical spinal decompression therapy: Does the scientific literature support efficacy claims made in the advertising media? Chiropractic & Osteopathy 15:7, May 18, 2007.
- Lee, Serafin. Outcomes of acute and chronic patients with magnetic resonance imaging-confirmed symptomatic lumbar disc herniation receiving high-velocity, low-amplitude spinal manipulation therapy: a prospective observational cohort study with one year follow-up. Journal of Manipulative and Physiologic Therapeutics 2014. doi 10.1016/j.jmpt.2013.12.011. http://www.jmptonline.org/article/S0161-4754(14)00034-7/abstract.
- Ernst CW, Stadnik TW, Peeters E, Breucq C, Osteaux MJ. Prevalence of annular tears and disc herniations on MR images of the cervical spine in symptom free volunteers. Eur J Radiol. 2005 Sep;55(3):409-14. Epub 2005 Jan 1.
- Dwain M Daniel, Non-surgical spinal decompression therapy: does the scientific literature support efficacy claims made in the advertising media?, Chiropr Osteopat. 2007; 15: 7.
- Pergolizzi, Joseph, Richmond, Charlotte, Auster, Martin, Florio, Frank and Wilhelm, Jonathan, Non-surgical Spinal Decompression for the Treatment of Chronic Low back pain – A Case Report, Spine-European Musculosckeletal Review, 2008;3(2) 58-60
- Olivero WC, Wang H, Hanigan WC, et al. Cauda equina syndrome (CES) from lumbar disc herniation. J Spinal Disord Tech 2009;22:202–6.
- Thomson S. Failed back surgery syndrome – definition, epidemiology and demographics. Br J Pain. 2013;7(1):56–59.
- Zafeer Baber and Michael A Erdek, Failed back surgery syndrome: current perspectives, J Pain Res. 2016; 9: 979–987.
This blog has been provided by Dr. John Coppola, D.C. and Dr. Valerie Monteiro, D.C. Dr. Coppola and Dr. Monteiro are the founders of the San Antonio Neuropathy Center, and Precision Sport & Spine. They specialize Herniated Disc Pain treatment They are the authors of the critically acclaimed book “Defeat Neuropathy Now …. In Spite of Your Doctor. The doctors have over 25 years of clinical experience.
If you would like to reach the doctors regarding a specific health problem, you may email them at [email protected].

 Over-the-counter medication (OTC): Ibuprofen- or naproxen-based drugs can help with mild to moderate pain. These should be used only short term. Chronic long term use can cause kidney disease.
Over-the-counter medication (OTC): Ibuprofen- or naproxen-based drugs can help with mild to moderate pain. These should be used only short term. Chronic long term use can cause kidney disease.
Comments are closed, but trackbacks and pingbacks are open.